更多案例:意外後的美學重建,一段從細節出發的植牙與全瓷冠治療
很多患者在諮詢時會問:「你們用哪一個牌子?」
品牌當然重要,但從長期追蹤的角度來看,造成差異的不只是品牌本身,更重要的往往是位置。
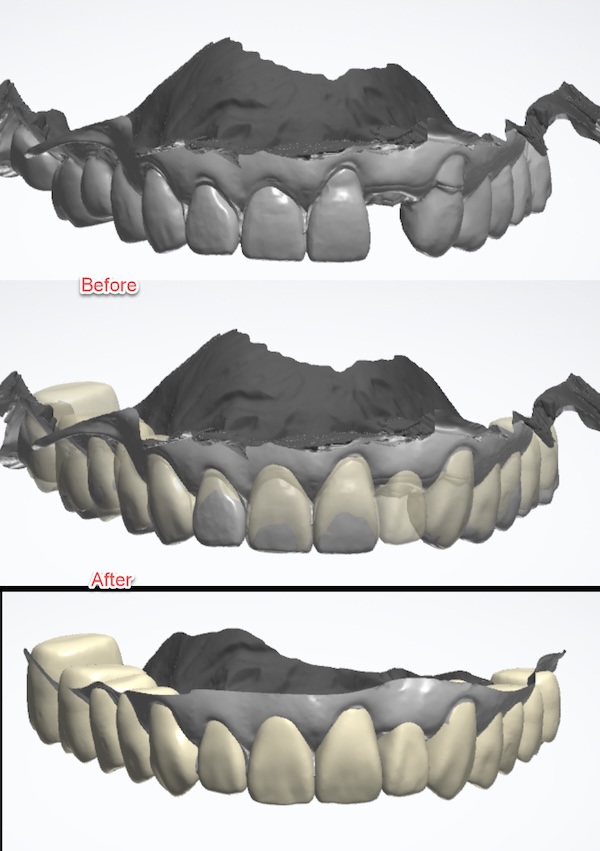
植牙的風險,多半不是來自大錯誤。
臨床上,我更常看到的是,許多小偏差累積而成的長期困擾:
‧ 深度「一點點」太深 → 清潔變難、牙齦易刺激
‧ 角度「一點點」不理想 → 受力不佳、假牙型態被迫妥協
‧ 清潔空間「一點點」不足 → 每天刷牙都變成挑戰
這些在短期可能看不出來,但五年十年後就會累積成大問題。
Many patients ask during consultations, “Which brand do you use?”
Brand matters—but from a long-term perspective, outcomes are shaped not only by the system itself, but even more by where the implant is placed.
Most implant failures don’t come from major mistakes. In clinical practice, they’re more often the result of small deviations that accumulate over time:
‧ a depth placed just a little too deep → harder to clean, more gum irritation
‧ an angle slightly off → compromised load distribution and forced prosthetic compromises
‧ just a bit too little cleaning space → daily hygiene becomes a challenge
These issues may be invisible in the short term, but five or ten years later, they often add up to significant problems.
📚 醫學研究怎麼看?(Evidence Box)
What Does the Evidence Show? (Evidence Box)
系統性回顧與統合分析指出,靜態電腦輔助導引植牙(static computer-aided implant surgery)在多數臨床情境下可達到臨床可接受的放置精準度。精準度的提升,能降低因位置偏差導致的修復妥協與維護困難。
Systematic reviews and meta-analyses indicate that static computer-aided implant surgery achieves clinically acceptable placement accuracy across most clinical scenarios. Improved accuracy helps reduce restorative compromises and long-term maintenance challenges caused by positional deviations.
參考文獻:Tahmaseb A., Wu V., Wismeijer D., Coucke W., Evans C. (2018)
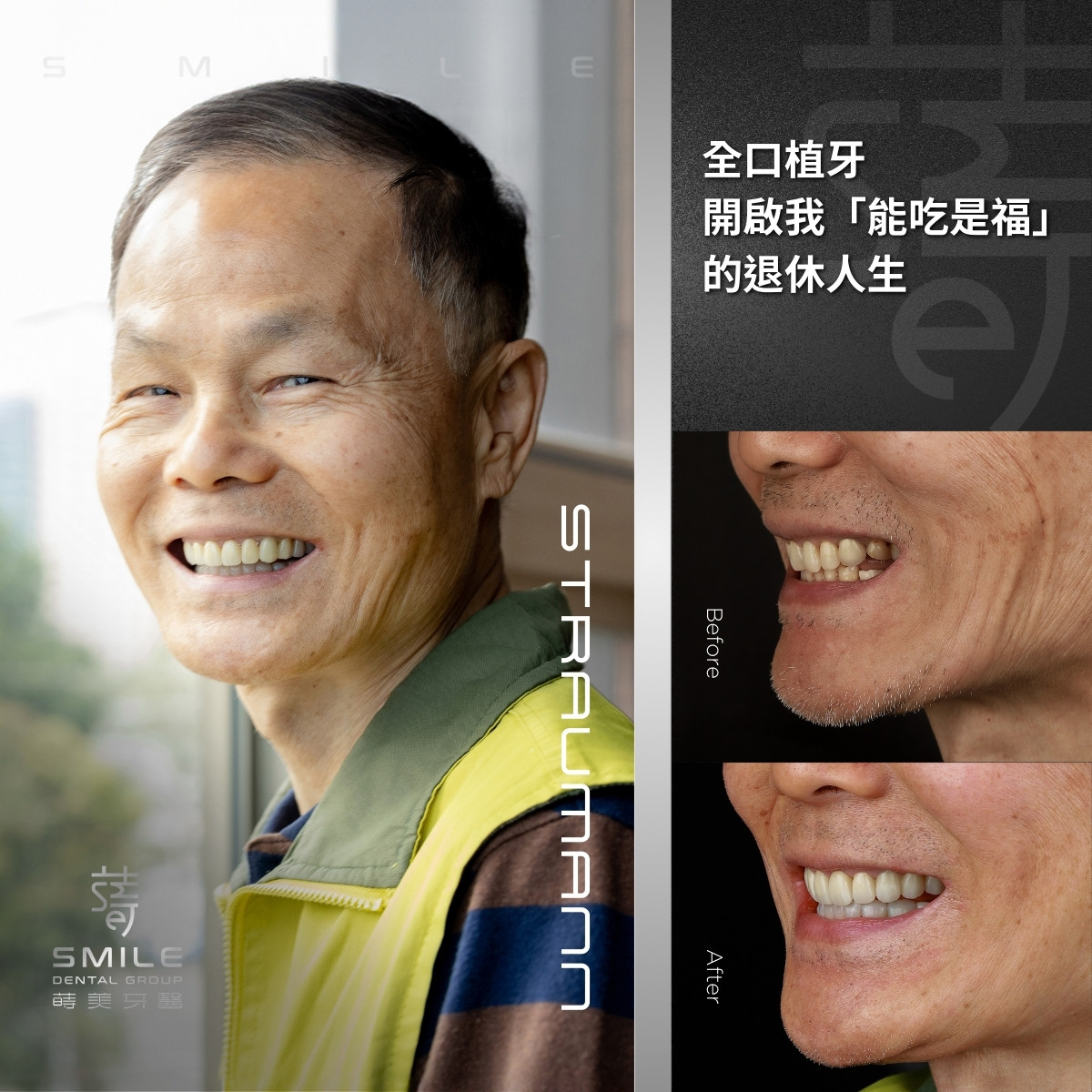
全數位規劃的核心:把植體放在「假牙與牙齦需要的位置」
The Core of Digital Planning: Placing the Implant Where the Crown and Gums Need It


現代數位流程不是科技炫技,而是把植牙的思考從「能不能放」,往前推進到「為未來使用而放」:
‧ CBCT 看骨頭三維結構
‧ 口掃看牙齒與牙齦形態
‧ 反向設計先確定最終牙冠、咬合、清潔路徑
‧ 需要時搭配導引,讓放置更可預期
為什麼這對 Tissue Level 特別重要?
因為 TL 的優勢是更友善牙齦的界面,但它必須被放在對的位置才能發揮。
用數位方式控制深度與清潔架構,才能真正把 TL 的設計優勢轉換成長期更穩定、更好維護。
Modern digital workflows aren’t about showcasing technology—they shift implant planning from “Can we place it?” to “Where should it be placed for long-term use?”
‧ CBCT defines the three-dimensional bone anatomy
‧ Intraoral scanning captures tooth and gingival form
‧ Reverse planning establishes the final crown, occlusion, and cleaning pathways first
‧ Surgical guides, when needed, help make placement more predictable
Why does this matter especially for tissue-level implants?
Because the advantage of TL lies in a gum-friendly interface—but only when the implant is placed correctly. Digital control of depth and hygiene architecture is what turns TL design into lasting stability and easier long-term maintenance.
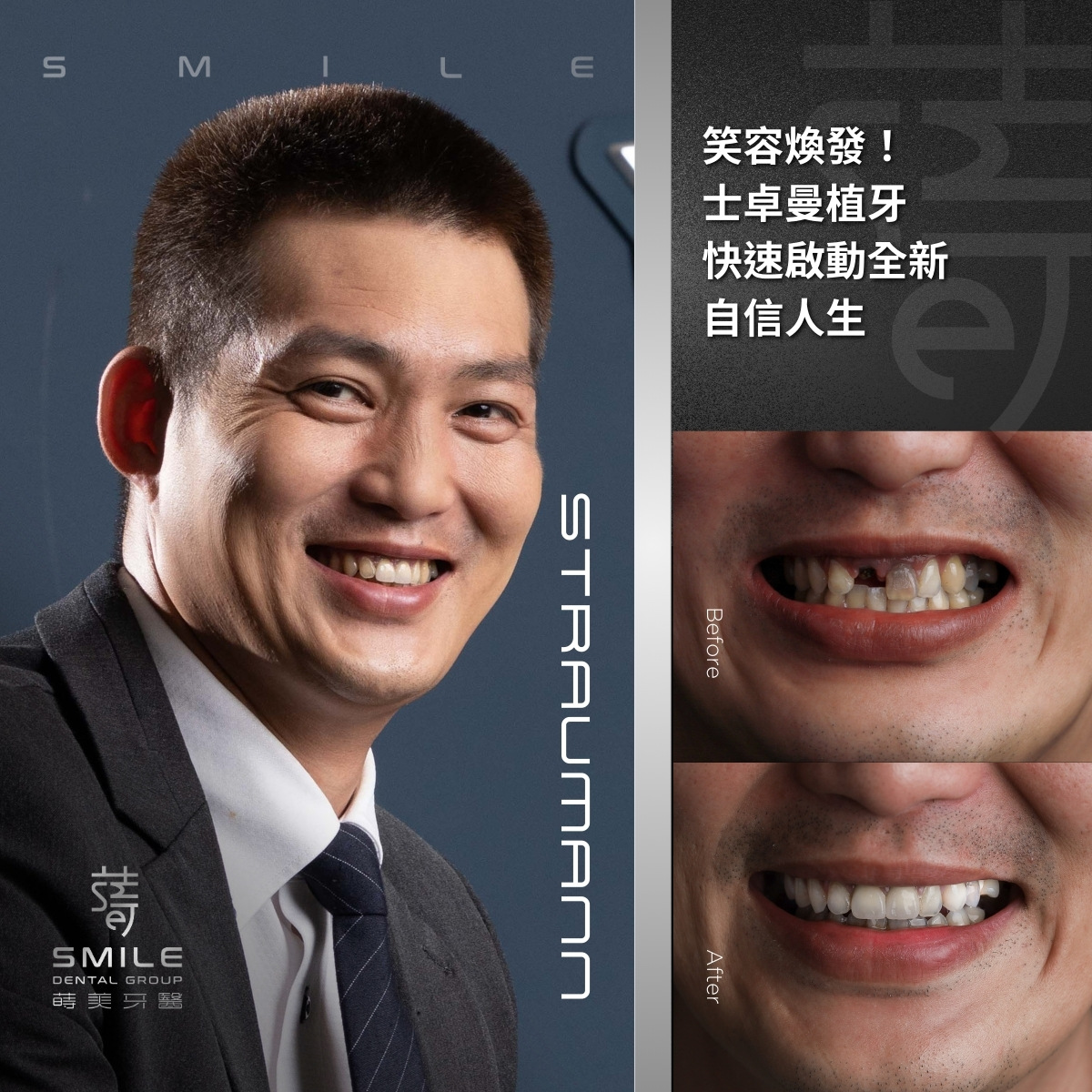
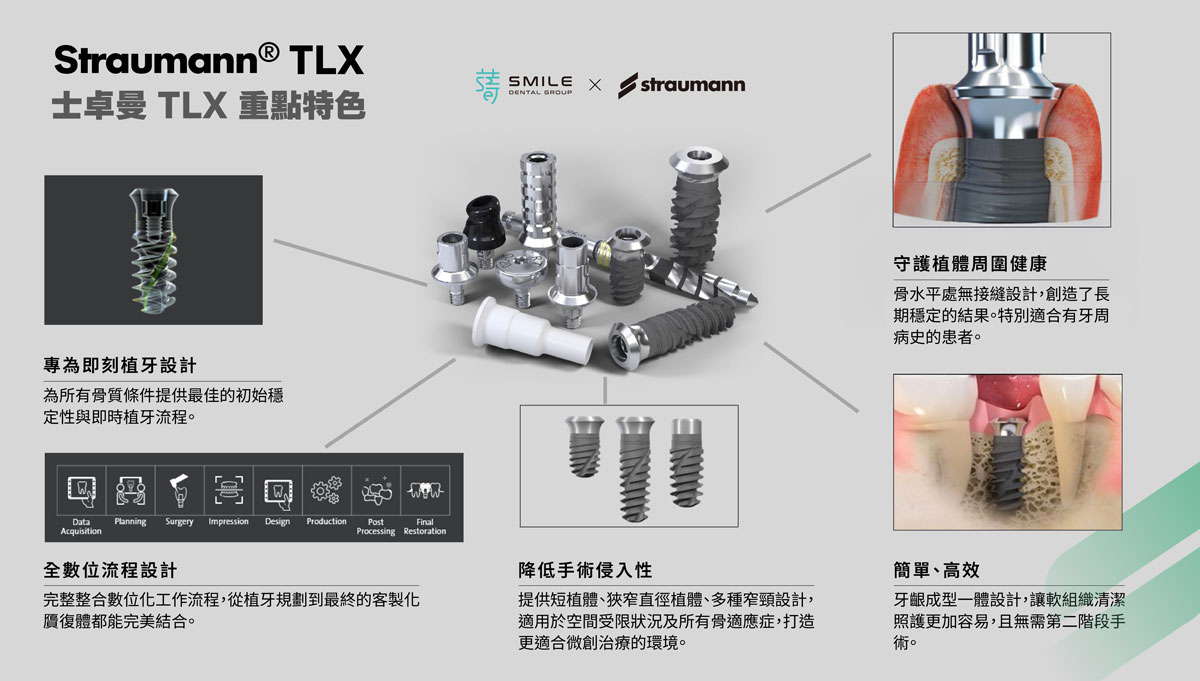
Straumann TL:為何同樣叫 Tissue Level,長期結果卻不同?
Straumann TL: Why Do Long-Term Outcomes Differ Even Among Tissue-Level Designs?
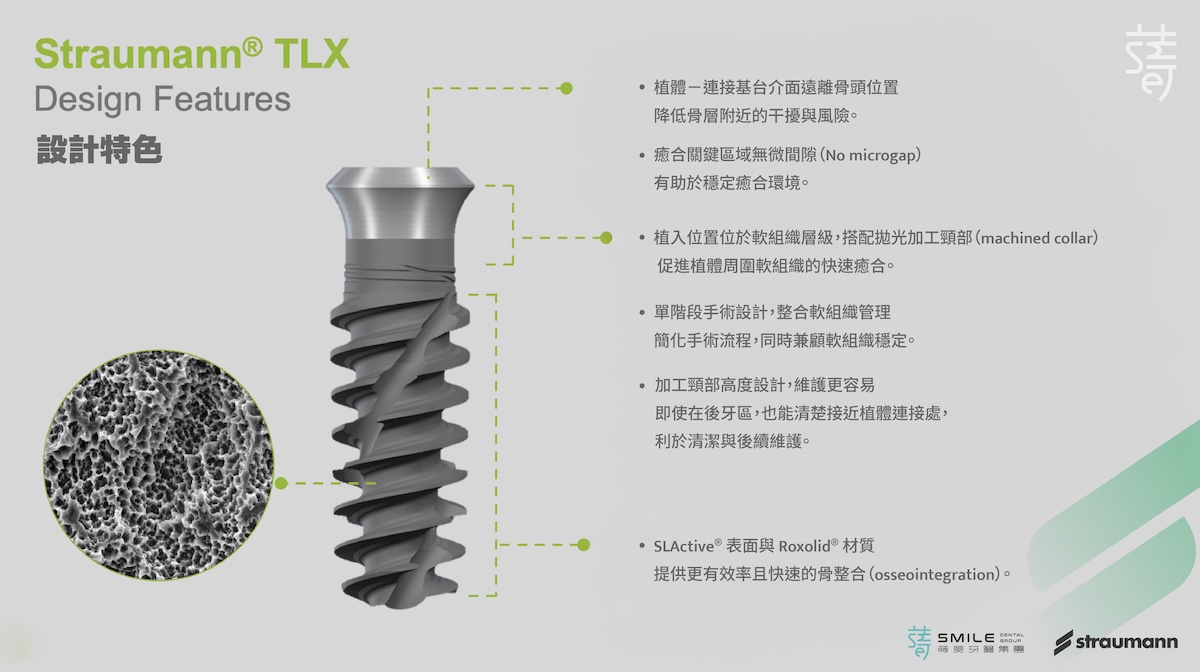
在選擇 Tissue Level 植體時,我會考量它是原生設計,還是延伸改造?
Straumann TL 的核心價值並不僅止於將接縫位置外移,而是從一開始就把相關設計圍繞著「風險外移」的原則,讓脆弱的牙齦組織,能在位置被精準控制的前提下,長期處在相對穩定、不受結構刺激的環境中。
這是設計哲學上的底層差異,而非僅僅是外觀形式的不同。
也因此,即使同樣被歸類為 Tissue Level 設計,不同系統在設計重點與風險承受度上,仍可能存在差異。這也解釋了為何在長期追蹤中,Straumann TLX 與 TLC 往往能在位置放對的情況下,展現出較為穩定、具備高度一致性的臨床表現。
When selecting a tissue-level implant, I look beyond the label to ask a more fundamental question: is this a native design—or an adaptation of a bone-level platform?
The core value of Straumann TL is not simply moving the junction outward. From the outset, its design is built around a single principle: shifting risk away from vulnerable tissues. By precisely controlling implant position, the system is intended to keep delicate gingival tissue in a more stable environment—less exposed to structural irritation over time.
This reflects a difference in design philosophy, not just appearance.
As a result, even though multiple systems may be categorized as tissue-level, their priorities—and tolerance for biological risk—can vary significantly. This helps explain why, in long-term follow-up, systems like Straumann TLX and TLC often demonstrate more stable and consistent clinical outcomes when placed correctly.