江政倫 醫師
金山蒔美總院長/板橋蒔美院長暨主治醫師/北大蒔美主治醫師/三重蒔美主治醫師/蒔美牙醫集團執行長
植牙成功,不只取決於骨頭。為什麼我更在意牙齦的長期穩定性?

在植牙諮詢時,患者最常問我的問題是:「骨頭夠不夠?」「需不需要補骨?」
這些問題都很重要,因為骨頭條件確實會影響植牙能不能做、是不是穩定。
但如果你問我:一顆植牙能不能真正用得久,我腦中第一個浮現的往往不是骨頭,而是牙齦。
骨頭條件是否足夠,影響的是手術當下的成功;但牙齦能否穩定,才是決定這顆牙,十年後還在不在、好不好清、會不會反覆發炎的重要關鍵。
In implant consultations, patients often ask whether there is enough bone, or if bone grafting will be needed. These are important considerations, as bone quality affects whether an implant can be placed successfully.
But when it comes to whether an implant will truly last, my first concern is not the bone—it’s the gums. Bone supports initial success; long-term gum stability determines whether that implant remains healthy, maintainable, and free of inflammation years down the line.
骨整合成功,為什麼仍可能在幾年後出問題?
If osseointegration is successful, why can problems still emerge years later?

現代植牙的骨整合成功率已經非常高,很多人手術後半年、一年回診時看起來都很穩定。
但臨床追蹤拉長後,你會發現不少問題其實是「慢慢累積」出來的:
‧ 牙齦反覆紅腫、刷牙流血
‧ 清潔不易、經常卡食物
‧ 口氣或味道變重
‧ X 光下邊緣骨逐年下降
這類狀況多半不是患者不夠努力配合,也不一定是植體鬆動,而是牙齦長期處於不好維護、容易被刺激的環境。
Modern dental implants achieve very high rates of successful osseointegration. At six months or a year after surgery, many implants appear stable.
But with longer follow-up, problems often emerge gradually: recurring gum inflammation and bleeding, difficulty keeping the area clean, food trapping, unpleasant odor, and progressive marginal bone loss on X-rays.
In most cases, these issues are not due to poor patient compliance or a loose implant, but to gum tissue that has been placed in an environment that is difficult to maintain and easily irritated over time.
植牙的第一道防線:不是骨頭,而是牙齦
The First Line of Defense in Dental Implants: Not Bone, but the Gums

天然牙有牙周韌帶,植體沒有。
這代表植體周圍的防護主要靠:周圍黏膜(peri-implant mucosa)形成的生物屏障。
一旦這個屏障反覆發炎、封閉不穩,影響就會逐步往深處走,最後仍會反映在骨頭上。
這就是我把「牙齦穩定」放在規劃第一順位的原因。
Natural teeth are supported by the periodontal ligament; implants are not.
That means an implant’s primary defense relies on the biological seal formed by the surrounding peri-implant mucosa. When this barrier is repeatedly inflamed or unstable, problems tend to progress deeper—and eventually show up as bone loss. This is why gum stability is my first priority in implant planning.
在規劃植牙時,我會先想三件事:
1.未來假牙形態與清潔路徑:刷牙、牙線、沖牙機是否好操作?
2.牙齦厚度與支撐:牙齦能不能長期維持高度、輪廓?
3.植體與結構轉換點的位置:讓牙齦接觸到什麼表面?有沒有不必要的刺激源?
這些問題如果在手術前沒有被設計好,後面再怎麼補救都會更辛苦。
When planning an implant, I focus on three things:
1. The future restoration and cleaning pathway: Can brushing, flossing, and irrigation be done easily?
2. Gum thickness and support: Can the soft tissue maintain its height and contour over time?
3. The implant–abutment transition: What surface will the gums contact, and are there avoidable sources of irritation?
If these factors aren’t designed before surgery, correcting them later becomes far more difficult.
📚 醫學研究怎麼看?(Evidence Box)
What does medical research show?
研究指出,植牙長期追蹤不能只看骨整合是否成功;植體周圍牙齦的發炎、出血、探診與封閉狀態,是影響長期穩定的重要指標。植體周圍的軟組織界面與天然牙不同,因此更需要以「維護友善」與「低刺激」的方式設計。
Research shows that long-term implant follow-up cannot focus on osseointegration alone. Inflammation, bleeding, probing depth, and the integrity of the peri-implant seal are critical indicators of long-term stability. Because the soft-tissue interface around implants differs fundamentally from that of natural teeth, it must be designed with maintenance in mind—prioritizing ease of care and minimal biological irritation.
為什麼我偏好 Tissue Level 的設計?(把風險往外移)
Why I Prefer Tissue-Level Implant Design: Moving Risk Outward
Tissue Level(TL)植體的核心價值不是「新」,而是它的結構讓牙齦接觸到較連續、穩定的頸部表面,並把結構轉換點(以及主要接合界面)相對外移,安排在較容易被觀察與清潔的位置。
The core value of tissue-level (TL) implants is not novelty, but structure. Their design allows the gums to interface with a more continuous, stable cervical surface, while shifting the structural transition—and the primary junction—outward to an area that is easier to see, monitor, and keep clean.
對患者而言,這通常帶來三個長期好處(在適當病例與良好維護前提下):
. 清潔更友善:較不容易形成深層死角
. 刺激更少:牙齦長期處於較穩定環境
. 維護更可預期:發炎風險更可被管理
For patients, this typically translates into three long-term benefits—when used in appropriate cases and supported by proper maintenance:
. More maintenance-friendly: fewer deep, hard-to-clean areas
. Less biological irritation: gums remain in a more stable long-term environment
. More predictable care: inflammation risks are easier to monitor and manage
但要說清楚:只有當植體被放在正確的位置時,TL 的設計優勢才能被完整發揮。
這也是為什麼我在臨床上把 TL × 全數位規劃 視為同一套策略:
TL 解決的是「牙齦生物學」,數位規劃解決的是「把它放在對的位置、對的深度、對的清潔架構」。
One thing is essential: tissue-level implants deliver their full benefit only when they are placed correctly.
That’s why I treat tissue-level design and digital planning as one strategy—one addresses soft-tissue biology, the other ensures proper position, depth, and long-term cleanability.
為什麼 Tissue Level 設計中,我選擇 Straumann?
Why I Choose Straumann for Tissue-Level Implant Design?
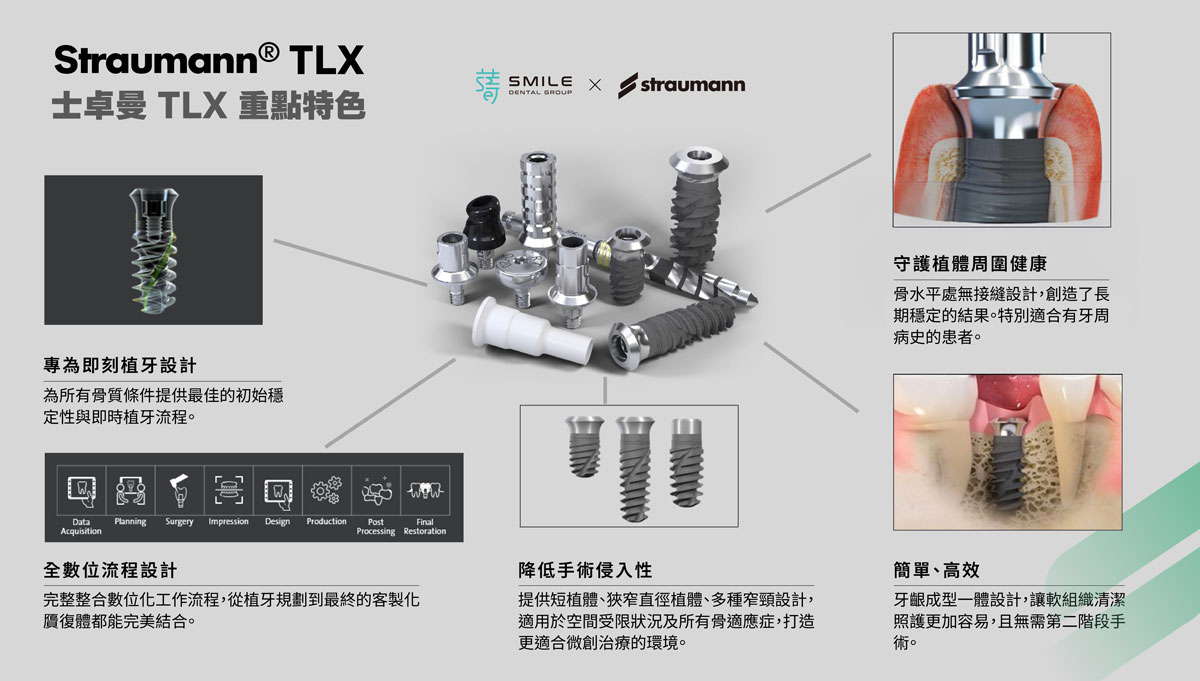
Straumann 作為 Tissue Level 植體的先驅,其 TL 系列涵蓋不同臨床世代與應用需求,包括 TLX 與 TLC 等代表性系統,皆源自相同的設計核心。
在相關學術研究中,已累積近 40 年的臨床追蹤數據。這些長期資料不僅提供穩定的醫學依據,也使 Straumann 在治療結果的穩定性與可預測性上,具備高度可信度。
因此,Straumann 的設計取向,更貼近我在臨床上所關切的重點:多年後是否仍能維持良好的治療成效。
As a pioneer of tissue-level implants, Straumann has developed a TL portfolio spanning multiple clinical generations and indications—including systems such as TLX and TLC—all built on the same core design principles. Backed by nearly 40 years of clinical follow-up, this body of evidence provides durable scientific support and lends Straumann a high degree of credibility for stable, predictable outcomes.
That long-term focus aligns closely with what matters most in my practice: whether results remain reliable years down the line.
江政倫醫師的臨床建議
Clinical Insight from Dr. Jiang Zhenglun


植牙不是做完就結束。它真正的考驗,是這個結構在多年後,能否持續被好好使用與維護。
評估治療時,除了關心「能不能做」,更重要的是了解:牙齦是否有被納入長期穩定規劃、植體放置位置是否為未來使用而設計、以及五年十年後的維護策略。
Dental implants don’t end when surgery is complete. Their real test is whether the structure can continue to be used—and properly maintained—years down the line.
When evaluating treatment, the question isn’t only whether an implant can be placed, but whether the gums have been planned for long-term stability, whether implant positioning is designed for future function, and how maintenance will be managed five or ten years from now.
如果你想更完整理解我們為什麼將 Tissue Level 植體 與 全數位植牙規劃流程 視為同一套長期策略,可以閱讀系列主頁〈為什麼我們將 Tissue Level 植體與全數位植牙流程結合?〉。
To better understand why we treat tissue-level implants and fully digital implant planning as a single, long-term strategy, you can explore our series overview, Why We Combine Tissue-Level Implants with a Fully Digital Implant Workflow.
References(醫師版)
‧ Salvi GE, Lang NP. Diagnostic parameters for monitoring peri-implant conditions. Int J Oral Maxillofac Implants. 2004.
‧ Lindhe J, Berglundh T. The interface between the implant and the soft tissues. J Clin Periodontol. 1998.